What You Need To Know About Gestational Diabetes
I never realized how controversial Gestational Diabetes Mellitus (GDM) could be…
As I dug into the research & talked with various professionals, I learned there are many different approaches to screening, diagnosing & treating GDM. In this post, I dive deep into the topic so you can make an informed decision & have a constructive dialogue with your healthcare team.
What is Gestational Diabetes Mellitus?
GDM is a type of diabetes that develops during pregnancy. Diabetes means your blood glucose (also called blood sugar) is too high. Elevated glucose in your blood is not good for you or your baby.
Elevated glucose levels during pregnancy are concerning & can lead to:
- mom having pre-eclampsia (hypertension) during pregnancy
- baby being born too early
- baby weighing too much at birth (macrosomia), which can make delivery difficult
- baby having low blood glucose (hypoglycemia) right after birth
- baby having breathing problems after delivery
Having GDM also puts mom & baby at higher risk for future health problems, including risk of developing type 2 diabetes later in life. Baby is also more likely to have obesity as a child or teen (1, 2).
What Causes Gestational Diabetes?
In addition to weight gain during pregnancy, your body’s hormones change. These changes influence your body’s ability to utilize insulin, a key hormone needed for blood glucose regulation, which can lead to insulin resistance. All pregnant women will experience some insulin resistance during late pregnancy. Luckily, most pregnant women are able to produce enough insulin to overcome any insulin resistance. However, women that cannot produce enough insulin during pregnancy, go on to develop GDM (1).
In addition to the changes a woman’s body encounters during pregnancy, there are other risk factors that predispose women to diabetes & GDM, including (2, 3).
- Overweight or obesity (BMI ≥25 kg/m2). Specially those with a history of cardiovascular disease, high blood pressure, low HDL cholesterol (<35mg/dL), or high triglycerides (>250mg/dL)
- Existing prediabates prior to pregnancy (HbA1c ≥5.7%)
- Previous pregnancy with GDM
- >25 years old (screening for diabetes is recommended for everyone over at 45 years)
- Women with a hormone disorder called polycystic ovary syndrome (PCOS)
- Gaining too much weight during pregnancy
- Having a family history of type 2 diabetes
- High-risk race/ethnicity (e.g. African American, Hispanic/Latino American, American Indian, Alaska Native, Native Hawaiian, or Pacific Islander
- Previously given birth to a baby weighing more than 9 pounds
- Physical inactivity
- Other clinical conditions associated with insulin resistance
Before getting pregnant, you may be able to prevent gestational diabetes by losing weight if you’re overweight, eating healthier, & getting regular physical activity.
The American Diabetes Association recommends screening & testing for Pre-diabetes & Type 2 Diabetes in women with one or more risk factors for type 2 diabetes at their initial prenatal visit using standard diagnostic criteria. Read the full paper here (3).
How is GDM diagnosed?
GDM is typically screened for &/or diagnosed during 24-28 weeks gestation in pregnant women who are not already known to have diabetes. A few organizations around the globe have slightly different approaches to diagnostic criteria & cutoff values. Different diagnostic criteria will identify different degrees of maternal hyperglycemia & maternal/fetal risk, leading some experts to debate on the optimal strategies for diagnosis.
There are two primary ways to test for & diagnose GDM.
One-step method.
The International Association of the Diabetes and Pregnancy Study Group’s (IADPSG) GDM diagnostic criteria includes a 1-step method –> referred to as the 75-g Oral Glucose Tolerance Test (OGTT) and is performed between 24-28 weeks gestation. The 75-g OGTT test is performed after an 8+ hour overnight fast, where 75-grams of glucose are administered to the patient (typically via a sweet tasting beverage). Plasma glucose levels are measured fasting, one & two hours after consuming the glucose. GDM is diagnosed when any of the following plasma glucose levels are met:
- Fasting: 92 mg/dL
- 1-hour: 180 mg/dL
- 2-hour: 153 mg/dL
It’s worth mentioning that the World Health Organization (WHO) & majority of organizations around the globe have adopted this method. However, the WHO guideline recommends conducting the OGTT any time during pregnancy (4).
Two-step method.
In 2013, The National Institutes of Health (NIH) convened a consensus panel with representatives from obstetrics/gynecology, maternal-fetal medicine, pediatrics, diabetes research, biostatistics & other related fields. The panel recommended a two-step approach to screening & diagnosis of GDM. This is the most common approach adopted in the United States.
First, a screen between 24-28 weeks gestation is conducted using a 1-hour 50-g glucose load test (GLT). If screened positive, a 3-hour 100-g OGTT is performed for diagnosis of GDM. It’s important to note the 50-g GLT screen does not need to be performed fasted, while the 3-hour 100-g OGTT does.
Below is a table, which outlines the diagnostic criteria using the 2-step method.
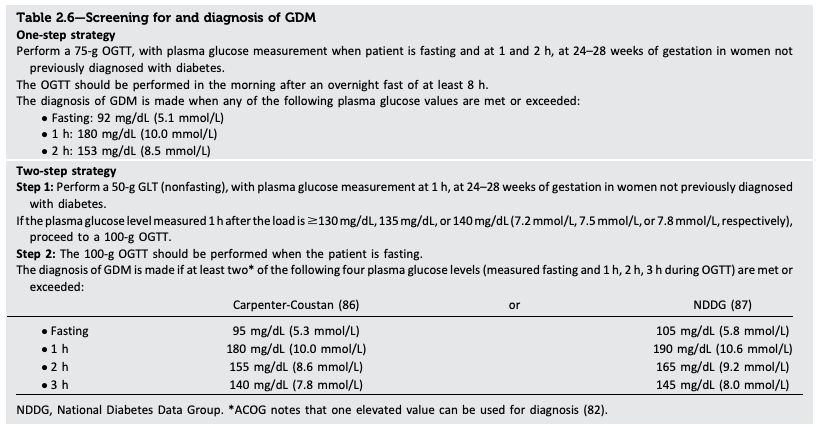
Source: Diabetes Care 2019 (3).
It’s important to note that various organizations may include their own take on the two-step screening approach & diagnostic criteria. The American College Of Obstetricians and Gynecologists (ACOG) currently supports the two-step method, but also mentions that one elevated value, as apposed to two, may be used for the diagnosis of GDM.
The American Diabetes Association (ADA) recommends the use of either the one-or two-step approach at 24-28 weeks in pregnant women not previously known to have diabetes. ADA also suggests that it may be advantageous to use the lower diagnostic thresholds shown in step 2 in the above table (3).
My Take
While data exists to support each strategy, I personally would choose & recommend the 1-step approach. There is evidence to support a correlation between maternal blood glucose levels & maternal/fetal consequences, thus a more conservative approach to screening & diagnoses would allow more women to know & manage their glycemia during pregnancy & beyond. I am also not a fan of the 50-g screen in the 2-step criteria. First, the screen does not capture fasted values & thus would eliminate women with high fasting glucose (such as myself) from being diagnosed with GDM. Second, the screen is not performed fasted, meaning a high-carb, high glycemic meal prior to the screen could potentially influence the screen & lead to a false positive.
Personal opinions aside, I also recognize the downside of universally adopting the 1-step approach. Use of the more conservative 1-step approach would increase the incidence of GDM, which may lead to “medicalization of GDM” through increased c-sections, increased intensive newborn assessments, & not to mention the increased life disruptions & psychosocial burdens on the diagnosed mother. Furthermore, many people are just not willing to change anything about their diet or lifestyle. Thus, more GDM diagnoses may not have much impact on health outcomes regardless. Discussion on cost-benefit, fetal/maternal outcomes, & future research are underway and much needed. I will continue to monitor the scientific advances & update my opinion as needed.
Are there alternatives for the screen & diagnostic test?
A common question I get is “do I really have to drink that sugary beverage?” The answer is not so black & white. While there are alternatives to the GLT screen & OGTT, most do not offer the same accuracy. That said, I strive to empower you with knowledge & options so you can make the best decision possible. Let’s look at a few alternatives.
- HbA1C screen. The use of the A1C screen at 24-28 weeks gestation does not function as well as the GLT. It’s a trade off between sensitivity & specificity (5). However, an A1C screen at your first prenatal visit may be a good idea (& is something I plan to request)!
- Home glucose-monitoring. This is my preferred method & one I opted for with my first pregnancy (but then ended having to take the 3-hour OGTT regardless…). There are downsides to this “testing” as it requires expert knowledge of a glucometer, is cumbersome, time-consuming, & results can be variable. I would only recommend this approach for someone who is highly motivated & has deep knowledge on diabetes & use of a glucometer.
I get it, the thought of drinking a highly concentrated “sugary beverage” is hard to swallow for a health-conscience mama. But let’s put it into perspective & see what 50-g of glucose actually translates to in real food.
50-g of pure close is 200 calories. Which roughly equates to:
-
-
-
-
- ~1/4 cup of white rice (dry)
- ~1.5 slices of white bread
-
-
-
*Note that 50-g equivalents will vary by brand.
I’ve seen some “experts” or midwifes recommend eating a banana, candy &/or juice in place of the 50-glucose beverage. Use caution with this approach as these foods are not necessarily equivalent to the glucose used in the GDM screen. Candy & fruit are not pure glucose, they contain other monosaccharide “sugars” like sucrose & fructose. The GLT screen has been standardized to a 50-g glucose load.
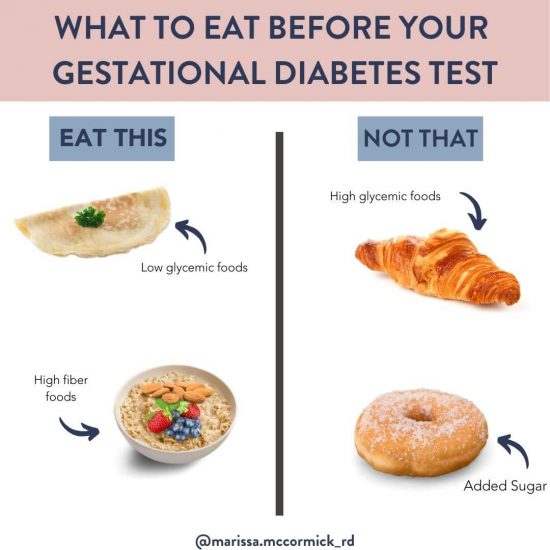
What should I eat before the 1-hour GDM screen?
For most women living in the United states, you’ll most likely endure the 50-g GLT screen for GDM sometime between 24-28 weeks of pregnancy (of course, you can discuss with your doctor the alternative options above). You do not need to take this test fasted. I recommend eating a well-balanced meal high in protein & fat 2-3 hours prior to the test. Keep the simple carbs in this meal low. If you do choose to eat carbs, choose high fiber carbs such as whole grains or fruit.
How is Gestational Diabetes managed?
If you happen to be diagnosed with GDM, you’ll likely be referred to a registered dietitian &/or certified diabetes educator. You’ll learn how to choose certain foods to help lower & stabilize your blood sugar, as well as how to increase your insulin sensitivity through exercise. You may also be trained to use a glucometer for at-home blood glucose readings. In some cases, you may need insulin injections.
Pregnancy blood glucose targets include (6):
- Fasting goal <95 mg/dL
- 1-hour goal of <140 mg/dL
.
Diabetes Postpartum Screen:
If you have GDM during pregnancy, you’ll be at increased risk for developing type 2 diabetes after delivery. The ADA recommends that women with GDM be tested 4-12 weeks postpartum for diabetes, using the 1-step method. Women with GDM should have lifelong screening for pre-diabetes/diabetes at least every 3 years (3).
Luckily, a well-balanced diet & physical activity is one of the best ways to prevent & manage type 2 diabetes. For tips on health meal prep & planning, head to this blog post or grab my FREE Nourished Mom’s Guide for tips on healthy meal prep & planning!
I know this is a lot of information packed into one post. If you’re not a dietitian or clinically trained professional, you may be feeling overwhelmed. I encourage you to read the post a few times & come prepared to have a robust dialog with your healthcare team. Your health, & the health of your baby, depend on it!
Helpful info. Fortunate me I discovered your website accidentally,
and I’m stunned why this coincidence did not happened in advance!
I bookmarked it.